Understanding Anesthesia Awareness: What You Need to Know
Awake during surgery is a rare but real medical phenomenon that affects approximately 1-2 out of every 1,000 patients undergoing general anesthesia. While the thought of being conscious during a procedure can be frightening, understanding the facts helps separate legitimate concerns from unnecessary fears.
Key Facts About Being Awake During Surgery:
- Anesthesia Awareness: Occurs in 0.1-0.2% of surgeries with general anesthesia
- Most Common During: Emergency procedures, C-sections, heart surgery, trauma operations
- Typical Experience: Brief moments of hearing sounds or feeling pressure, rarely pain
- Prevention: Modern monitoring equipment and skilled anesthesiologists drastically reduce risk
- Planned Awake Procedures: Many cosmetic and minor surgeries are safely performed with patients awake using local anesthesia
The confusion often stems from mixing up unintended awareness (waking up when you shouldn’t) with planned awake procedures (staying conscious by design). Emergency situations account for most awareness cases, while elective cosmetic procedures using local anesthesia or twilight sedation are entirely different experiences.
Understanding these distinctions helps you make informed decisions about your care and reduces anxiety about upcoming procedures.
As Dr. Sarah Yovino, I’ve spent years perfecting techniques for awake during surgery procedures, particularly in cosmetic treatments where patients benefit from staying conscious during their change. My background in pain management allows me to ensure patient comfort while maintaining the precision that conscious procedures offer.
Awake during surgery glossary:
What is Anesthesia Awareness?
Anesthesia awareness is when someone becomes conscious during surgery while they’re supposed to be completely “under” general anesthesia. It’s also called intraoperative awareness, and while it sounds absolutely terrifying, it’s incredibly rare – happening in only 1-2 out of every 1,000 surgeries.
Think of general anesthesia as hitting your brain’s “off switch.” It’s not like falling asleep naturally. Instead, it’s more like a reversible coma that prevents your brain from processing pain signals or forming memories. The goal is complete unconsciousness with no memory of what happened.
When awake during surgery unexpectedly occurs, the experience varies dramatically from person to person. Some patients remember vague, dream-like moments, while others have crystal-clear memories of specific conversations or events in the operating room.
The most common experiences include hearing sounds or conversations, feeling pressure or vibrations, and sensing an inability to move or communicate. The paralysis feeling is particularly distressing because muscle relaxants given during general anesthesia prevent patients from signaling that they’re aware.
Here’s some reassuring news: most patients who experience anesthesia awareness don’t feel actual pain, though the psychological impact can be significant.
What does it feel like to be awake during surgery?
Imagine being fully conscious but completely unable to move, speak, or signal for help. That feeling of helplessness is what makes anesthesia awareness so distressing, even when there’s no physical pain involved.
Some patients describe vague, dream-like states where they’re not entirely sure what’s real. Others have crystal-clear memories of hearing the medical team talking or feeling specific sensations during their procedure.
The experience might include hearing conversations about everyday topics, feeling pressure or tugging sensations, or becoming aware of bright lights. The inability to move or communicate – caused by the same medications that help surgeons work safely – can create intense anxiety and feelings of panic.
The psychological impact often extends far beyond the operating room. Many patients develop severe anxiety, nightmares, or even post-traumatic stress disorder (PTSD) after experiencing unexpected awareness during surgery.
If you’ve experienced anesthesia awareness or want to connect with others who have, the Anesthesia Awareness Campaign provides patient stories and support resources to help you understand you’re not alone in this experience.
Causes and Risk Factors for Waking Up During Surgery
Understanding why someone might become awake during surgery helps both patients and medical professionals work together to prevent this rare occurrence. While anesthesia awareness affects less than 0.2% of patients, certain factors can increase the likelihood of it happening.
The most common cause of anesthesia awareness is insufficient anesthetic dosage. This doesn’t mean your anesthesiologist made an error – sometimes they must carefully balance keeping you unconscious with keeping you safe. Your body might process anesthetic drugs faster than expected, or you might have a naturally higher tolerance to these medications.
Equipment malfunction is extremely rare thanks to rigorous safety checks, but it can occasionally affect anesthetic delivery machines or monitoring devices. Modern operating rooms have multiple backup systems to prevent these issues.
Your unique patient metabolism and genetic factors play a significant role too. Some people naturally require higher doses of anesthetics to stay unconscious. Interestingly, research shows that people with red hair often need more anesthetic medication than others – it’s all in the genes!
High-risk surgeries create the most challenging situations for anesthesiologists. During emergency surgery, there’s less time to assess your medical history and plan the perfect anesthetic approach. C-sections require lighter anesthesia to protect the baby, while heart surgery and trauma surgery often involve patients whose bodies can’t handle deeper levels of anesthesia without compromising their vital functions.
If you’ve had heavy alcohol or drug use, your body may have developed a tolerance that affects how anesthetics work. This isn’t about judgment – it’s about keeping you safe and comfortable during your procedure.
Who is at a higher risk of being awake during surgery?
Being honest with your anesthesiologist about your medical history is your best protection against awareness. Some factors that increase your risk include having experienced awareness before, which slightly raises the chances it could happen again.
Emergency situations carry the highest risk because medical teams must work quickly to save lives. Previous awareness history is important to discuss, as is daily alcohol consumption which can change how your body processes anesthetic drugs.
Patients with significant heart or lung problems may need lighter anesthesia to avoid dangerous complications. Emergency or trauma surgeries can have awareness rates as high as 10-40% in some studies because saving your life takes priority over perfect anesthesia depth.
The good news? Your anesthesiologist is trained to balance all these factors expertly. They use advanced monitoring equipment and their extensive knowledge to keep you both safe and unconscious throughout your procedure.
The Lasting Impact and How It’s Managed
Being awake during surgery when you’re not supposed to be can leave deep emotional scars that go far beyond the operating room. Even though the physical experience may be brief, the psychological impact can last for months or even years.
The most serious consequence we see is Post-Traumatic Stress Disorder (PTSD). This isn’t just feeling upset about what happened – it’s a genuine medical condition that affects how your brain processes the traumatic memory. Patients often develop persistent anxiety that makes everyday activities feel overwhelming. Nightmares become a nightly battle, replaying the helpless feeling of being trapped and unable to move.
Many people experience vivid flashbacks where they suddenly feel like they’re back in that operating room, hearing those same voices or feeling that same terror. This can happen anywhere – at the grocery store, during a family dinner, or while trying to fall asleep.
Perhaps most concerning is when patients develop medical phobias so severe that they avoid necessary healthcare. The thought of another procedure becomes unbearable, even for routine check-ups. Some people also struggle with depression and insomnia, as their trust in medical care has been shaken to its core.
What to do if it happens
If you think you were awake during surgery, please speak up immediately. Tell your surgeon, anesthesiologist, or any member of your medical team as soon as possible after your procedure. Don’t worry about whether your memories seem “real enough” or if you’re being dramatic – your experience matters.
Share every detail you can remember – the conversations you heard, any sensations you felt, or even just the overwhelming fear. This information helps your medical team understand exactly what happened and prevents it from occurring again.
Many patients feel tremendous relief just having their experience acknowledged and explained. Your doctor isn’t going to dismiss your concerns or make you feel foolish. We understand how frightening this must have been.
For those dealing with ongoing anxiety, nightmares, or other symptoms, professional counseling can make a world of difference. Therapists who specialize in trauma, particularly those trained in cognitive-behavioral therapy or EMDR, have excellent success helping people process these experiences. Support groups also provide a safe space to connect with others who truly understand what you’ve been through.
Consider contributing your experience to the Anesthesia Awareness Registry at the University of Washington. Your story helps researchers better understand this rare complication and develop even better prevention strategies.
Signs and Symptoms of Anesthesia Awareness
Recognizing anesthesia awareness can be tricky because it’s supposed to be impossible – you should be completely unconscious. But there are telltale signs that something has gone wrong, both from what you might remember and what your medical team observes.
From your perspective, the most terrifying part is usually the complete inability to move or speak. The muscle relaxants used during surgery mean you can’t signal for help, even though you’re desperately trying. Many patients remember hearing specific conversations – sometimes medical discussions about their procedure, other times casual chatter between team members.
You might recall feeling pressure, pulling, or vibration rather than sharp pain. Some people describe it as feeling the surgery happening “to” them but not necessarily hurting. Others experience a profound sense of panic and helplessness, knowing something is terribly wrong but being powerless to do anything about it.
These memories can be crystal clear or dream-like, and sometimes they don’t surface until days or weeks later when something triggers the recall.
From your anesthesiologist’s viewpoint, there are warning signs that might indicate you’re too lightly anesthetized. Your heart rate might suddenly spike without explanation, or your blood pressure could jump unexpectedly. Some patients start tearing up or sweating even though they appear unconscious.
Rarely, if the muscle relaxants are wearing off, you might make small movements, swallow, or grimace. Your pupils might dilate in response to stress.
The challenge is that these same signs can happen for other reasons – blood loss, surgical stimulation, or underlying health conditions. That’s why anesthesiologists use sophisticated monitoring equipment alongside their clinical experience to keep you safely unconscious throughout your procedure.
How Anesthesiologists Prevent You from Being Awake During Surgery
Preventing unintended awake during surgery experiences is truly an art and science combined. Modern anesthesiologists, including Dr. Justin Yovino, are medical detectives who specialize in keeping you safe, comfortable, and completely unaware during procedures that require general anesthesia.
The journey to safe anesthesia begins long before you enter the operating room. During your pre-operative assessment, your anesthesiologist becomes your personal safety advocate, diving deep into your medical history like a careful investigator. They want to know everything – your previous surgeries, any unusual reactions to medications, your current prescriptions, and yes, even those herbal supplements you might think are “no big deal.”
This isn’t just paperwork – it’s precision planning. Every detail helps create a customized anesthesia plan that’s as unique as you are. Think of it as creating a recipe where getting the measurements exactly right makes all the difference.
Once you’re in the operating room, the real magic of modern monitoring begins. Your anesthesiologist becomes your personal guardian, watching over multiple vital signs simultaneously. Your heart rate and rhythm are tracked through continuous electrocardiogram monitoring, while blood pressure measurements ensure your cardiovascular system stays stable. Oxygen saturation monitoring confirms your blood is carrying enough oxygen, and breathing rate and carbon dioxide levels verify that ventilation is working perfectly.
But here’s where technology gets really impressive. Brain function monitors like the Bispectral Index (BIS) actually measure your brain’s electrical activity and translate it into a number. For general anesthesia, anesthesiologists aim to keep this number between 40 and 60 – a sweet spot that indicates deep, comfortable unconsciousness. It’s like having a window into your brain’s activity level.
Another crucial tool is monitoring End-Tidal Anesthetic Concentration (ETAC), which shows exactly how much anesthetic gas your body is absorbing. This allows for precise, real-time adjustments to keep you at the perfect level of unconsciousness.
The most important element isn’t a machine at all – it’s your anesthesiologist’s clinical expertise. Years of training and experience allow them to interpret all this data together, making split-second decisions based on your individual needs. The latest research on preventing awareness continues to refine these techniques, making anesthesia safer than ever.
Your Role in Reducing the Risk
While your anesthesiologist leads the safety charge, you’re actually a crucial team member in preventing awake during surgery experiences. Think of yourself as the key witness who holds vital clues to your own safety.
Full disclosure is your superpower here. Share your complete medical history, including any family stories about unusual reactions to anesthesia. Sometimes genetic factors can affect how your body processes anesthetic drugs, and this family history can be incredibly valuable.
All medications matter – and we mean all of them. That includes prescription drugs, over-the-counter pain relievers, herbal supplements, vitamins, and yes, recreational substances too. Some patients worry about judgment, but remember – your anesthesiologist has heard it all and cares only about keeping you safe. Certain substances can dramatically change how your body responds to anesthetics, potentially requiring higher doses to maintain unconsciousness.
Allergies need to be crystal clear. Even reactions that seem minor or unrelated can influence which medications are safest for you.
Previous anesthesia problems are like red flags that help your anesthesiologist prepare extra safeguards. If you’ve experienced awareness before, or if family members have had unusual reactions, this information allows for additional monitoring and precautions.
Alcohol and drug habits significantly impact anesthetic requirements. Regular alcohol consumption can increase your tolerance to anesthetic agents, meaning you might need higher doses to stay unconscious. Being honest about these habits isn’t about judgment – it’s about mathematics and safety.
Most importantly, communicate your fears. If the thought of being awake during surgery terrifies you, say so. Your anesthesiologist wants you to feel confident and secure. They can explain exactly what they’re doing to prevent awareness and may even use additional monitoring techniques for extra peace of mind.
This is truly a team effort. Your honesty combined with modern monitoring technology and expert medical care creates the safest possible environment for your procedure.
Awake by Design: When Being Conscious During Surgery is the Plan
There’s a world of difference between accidentally waking up during surgery and choosing to stay awake for your procedure. Understanding this distinction can transform your perspective on awake during surgery options and help you make informed decisions about your care.
When we talk about planned awake procedures, we’re discussing a completely different experience from unintended anesthesia awareness. These procedures are carefully designed around your comfort and safety, using targeted anesthesia that numbs only the areas being treated while keeping you conscious and comfortable.
Think about it this way: when you get a filling at the dentist, you’re awake during a surgical procedure, but it doesn’t feel scary or dangerous. That’s because your dentist uses local anesthesia to block pain signals from that specific area. Modern cosmetic procedures work on the same principle, just with more sophisticated techniques.
The key differences are striking. With unintended awareness during general anesthesia, patients experience unexpected consciousness, often with feelings of paralysis and helplessness. In contrast, planned awake procedures involve conscious participation, complete pain control in the surgical area, and the ability to communicate with your medical team throughout the experience.
| Feature | Unintended Anesthesia Awareness (General Anesthesia) | Planned Awake Procedures (Local/Regional/Sedation) |
|---|---|---|
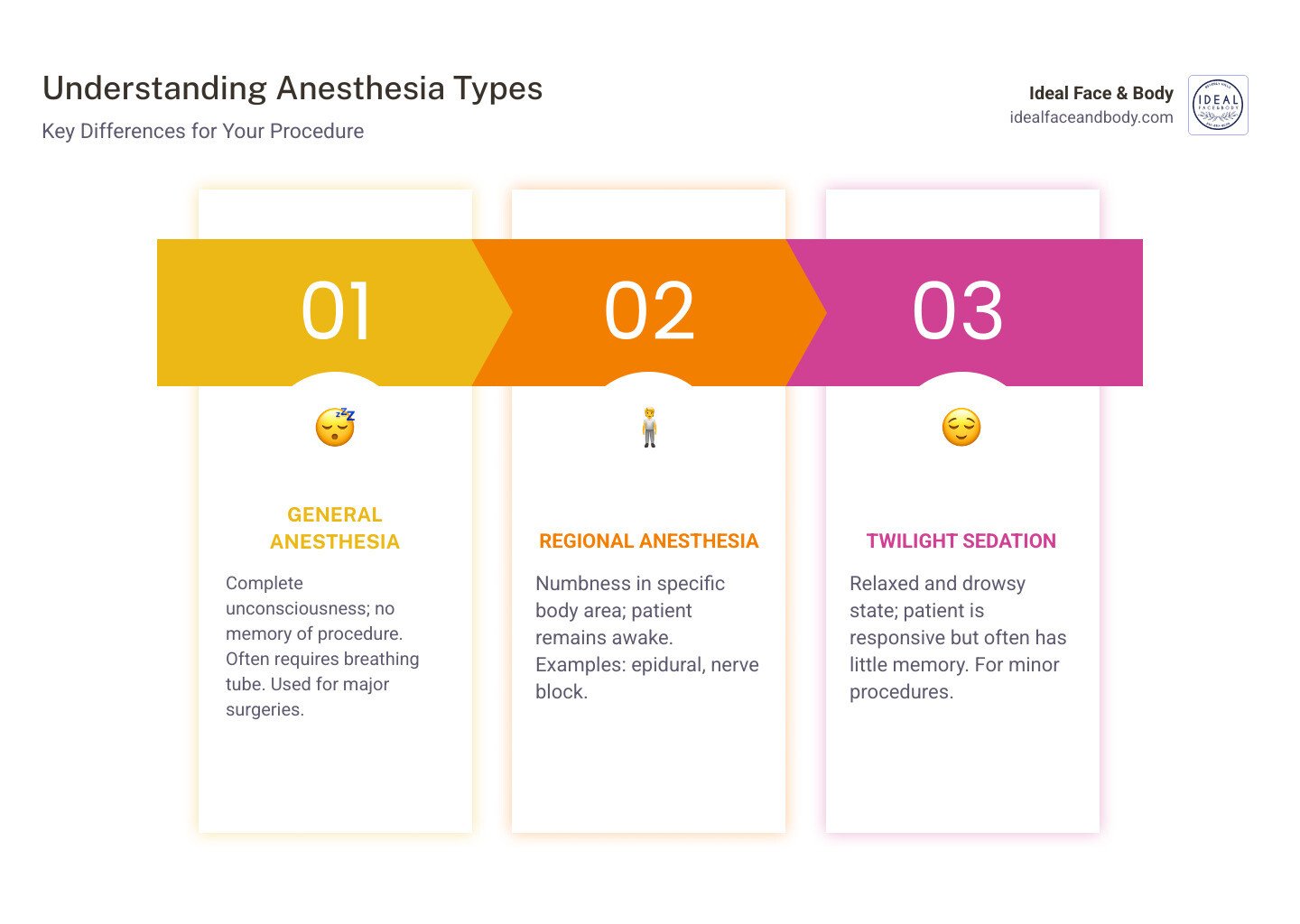
| Anesthesia Type | General Anesthesia | Local, Regional (Epidural, Nerve Block), Sedation |
| Patient State | Unintended consciousness during expected unconsciousness | Conscious, alert, or lightly sedated |
| Sensation | Can include hearing, pressure, rare pain, paralysis | Numbness in surgical area, no pain, can feel touch/pressure |
| Goal | Complete unconsciousness and amnesia | Pain control, patient comfort, sometimes patient cooperation |
| Recovery | Can be traumatic, potentially long-term psychological effects | Faster, less post-anesthesia side effects, quicker return to normal activity |
| Risk | Rare but serious complication | Generally low risk, custom to procedure and patient |
Many everyday medical procedures happen with patients fully awake and comfortable. Colonoscopies often use twilight sedation, where you’re drowsy but responsive, with little to no memory of the procedure afterward. Various biopsies, from skin samples to needle biopsies, typically require only local numbing. Even complex orthopedic procedures like hand and wrist surgeries are increasingly performed using regional nerve blocks combined with light sedation.
The world of cosmetic surgery has acceptd these advanced awake techniques with remarkable success. At Ideal Face & Body, we’ve perfected procedures like Precision Sculpt awake liposuction, where patients remain conscious and comfortable throughout their change. This approach offers several advantages: you avoid the risks associated with general anesthesia, experience faster recovery times, and often feel less post-operative nausea or grogginess.
Our patients frequently tell us they appreciate being able to participate in their aesthetic journey. There’s something empowering about being awake and aware during your procedure, knowing exactly what’s happening and being able to communicate with Dr. Sarah Yovino and our team throughout the process.
The safety profile of these planned awake procedures is excellent when performed by experienced professionals. The anesthesia is targeted specifically to the treatment area, your vital functions remain completely normal, and you maintain control over your breathing and other bodily functions.
Whether you’re considering awake liposuction, a painless lip augmentation, or another cosmetic procedure, the key is choosing a practice with experience in these advanced techniques. The comfort and safety of awake during surgery procedures depend entirely on the skill and expertise of your medical team.
Conclusion
We hope this comprehensive guide has helped ease your concerns and provided clear, factual information about awake during surgery. The bottom line is this: unintended anesthesia awareness is exceptionally rare, affecting fewer than 2 out of every 1,000 patients. Modern anesthesia has evolved into one of the safest aspects of medical care, thanks to remarkable advances in medications, sophisticated monitoring equipment, and the expertise of skilled anesthesiologists like Dr. Sarah Yovino and Dr. Justin Yovino.
The key to preventing awareness lies in teamwork between you and your medical team. Your role is simple but crucial: be completely honest about your medical history, medications, previous anesthesia experiences, and lifestyle habits. This open communication allows your anesthesiologist to create a personalized plan that keeps you safe and comfortable throughout your procedure.
What’s equally important to understand is that many awake during surgery procedures are intentionally designed that way – and for good reason. These modern techniques offer significant advantages, including faster recovery times, fewer side effects, and often better surgical outcomes. At Ideal Face & Body in Beverly Hills, CA, we’ve acceptd these advanced awake techniques because they allow our patients to experience their change in comfort while maintaining complete control over their experience.
Our expertise in Precision Sculpt awake liposuction and painless aesthetic procedures represents the future of cosmetic surgery. By choosing awake procedures, you’re not only avoiding the risks associated with general anesthesia but also enjoying a more personalized, comfortable experience with quicker recovery times.
Knowledge is power. The more you understand about anesthesia and surgical options, the more confident you’ll feel about your healthcare decisions. Whether you’re considering a major surgery requiring general anesthesia or exploring the benefits of awake cosmetic procedures, you now have the facts to make informed choices.
Learn more about Awake Liposuction in Beverly Hills, CA and find how our innovative techniques can help you achieve your aesthetic goals safely and comfortably.